A recent study has given evidence to suggest that a popular antimicrobial additive plays a part in inducing bacterial tolerance to some of our most powerful antibiotics.
The research, which was carried out by microbiologists at Washington University, Corey Westfall and Petra Levin and is still in the peer-review stage of publication, showed that bacteria grown in the presence of triclosan showed a greater ability to survive when they were subsequently exposed to a panel of antibiotics than their wild-type counterparts.
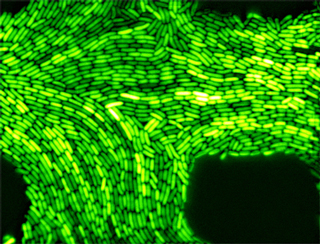
Bacteria can become tolerant to the effects of an antibiotic drug when they become persister cells – what this means is that the bacterial cells exist in a kind of ‘limbo’, or dormant state. Essentially, this means that they aren’t metabolically active anymore and won’t grow, but are still able to hang around. With less chemical processes happening which the antibiotics could use as a target, the persister bacterial cells become tolerant to the drug’s action.
Triclosan is an antimicrobial additive that works by stopping bacteria from growing – in other words it’s a bacteriostatic drug. It’s used in a huge range of products including cleaning supplies, shampoo, toothpaste and mouthwash, to name a few. It’s even used widely in consumer products like toys and beauty products. The fact that it’s used so much has led to questions being asked about the role it’s playing in encouraging antibiotic resistance. In fact, the US Food and Drug Administration has banned triclosan from being included in consumer soaps, starting September 2017.
The research team conducted the study after raising the question whether triclosan’s bacteriostatic action could help protect bacteria from bactericidal drugs, those that require their bacterial target to be metabolically active, and work by outright killing the bacteria.
To test if this was the case, they grew Escherichia coli and methicillin resistant Staphylococcus aureus (MRSA), both in the presence of triclosan and without, and then exposed these bacteria to a panel of antibiotics for 20 hours.
They found that triclosan was able to help protect E. coli against the action of four antibiotics. Survival of the bacteria was increased 1000-fold against kanamycin and 10,000-fold against streptomycin and ciprofloxacin when they were grown with triclosan. E. coli was also almost totally protected against the antibiotic ampicillin, with viable cells still showing up after 20 hours of exposure.
They were also able to show that MRSA exposed to triclosan showed increased survival against vancomycin. The paper notes that although the difference in viable cell count between MRSA grown with triclosan and MRSA grown without the additive wasn’t statistically significant, it still suggested that the bacterial cells were in a persister state.
The protective effect that triclosan seems to have on MRSA against vancomycin is especially worrying – vancomycin is often used as a last line of defence to treat MRSA when no other antibiotics are working. If triclosan could stop even this antibiotic from working, patients diagnosed with this infection could be at a much greater risk.
Corey Westfall and Petra Levin state that they aren’t sure exactly how triclosan could be causing this protective effect. Triclosan stops bacterial cells from growing by interfering with fatty acid synthesis, and they mention that this effect is linked to the emergence of a signal molecule called ppGpp, which in turn is implicated in antibiotic tolerance.
The results of the study should bring into light the risk we face in the massive overuse of triclosan, and hopefully will lead into further analysis of the potential effect this antimicrobial additive could have on our health.
