The bacterial species Klebsiella may contribute to a dangerously high level of antibiotic resistance in Kenya, a recent study suggests.
Published in the journal PLOS ONE, the study is a collaborative effort between institutions including the US Naval Research Laboratory (NRL) and the Kenya Medical Research Institute (KEMRI).
In many developing nations, the occurrence of antibiotic resistance can be fairly high for several reasons, such as the overuse of antibiotics, which promotes the emergence of resistant bacterial strains, and inefficient infection control procedures.
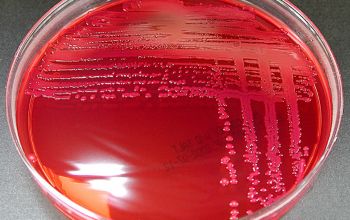
After testing intestinal samples from healthy individuals and patients suffering from diarrhoea in Western and Central Kenya, the study found a startling number of resistance genes in Klebsiella pneumoniae and K. oxytoca isolates.
Klebsiella species can be commonly found in the intestines, where they co-exist with other commensal intestinal bacteria. As they have been shown to acquire and pass on antimicrobial resistance genes to other bacterial species, a concern is that these intestinal Klebsiella could act as a resistance ‘reservoir’.
To examine this potential threat, the team obtained samples from eight different Kenyan medical clinics, and used these to isolate 90 Klebsiella strains. An NRL-developed microarray machine was used to identify genes which grant resistance to several key antibiotics, such as the aminoglycosides and macrolides.
It was found that 36.7% of the isolates were resistant to at least three of the antimicrobial classes, meaning that they would be considered multi-drug resistant. One isolate in particular showed extensive drug-resistance, with genes granting immunity to at least one agent in almost all classes.
Interestingly, the results showed that a significant number of isolates were resistant to tetracycline and trimethoprim/sulfamethoxazole (SXT), two drugs widely used in Kenya.
“These results suggest that there is a selective pressure for the establishment and maintenance of resistant strains,” said Dr. Chris Taitt, from the NRL Center for Bio/Molecular Science and Engineering. “This is potentially due to agriculture and prophylactic use of antibiotics, and further suggests the need for more effective public health policies and infection control measures than those currently implemented.”